Wisdom teeth, the dreaded pain that you don’t ever want to deal with. Wisdom teeth, also known as your third molars – reside at the back most region of your mouth, bringing the total number of teeth in your mouth to 32. Wisdom teeth come through at a much later age than the rest of your permanent teeth. The average age for wisdom teeth to erupt are around 18-25 years old, however, this can vary and, in some cases, they may never erupt or potentially erupt at a much later age. The eruption of wisdom teeth in the mouth are often associated with an unpleasant pain which can affect eating, talking and chewing. In most cases, the pain will disappear after the wisdom tooth has erupted ‘enough’. Others may not be so lucky and may suffer from persistent issues that require further intervention.
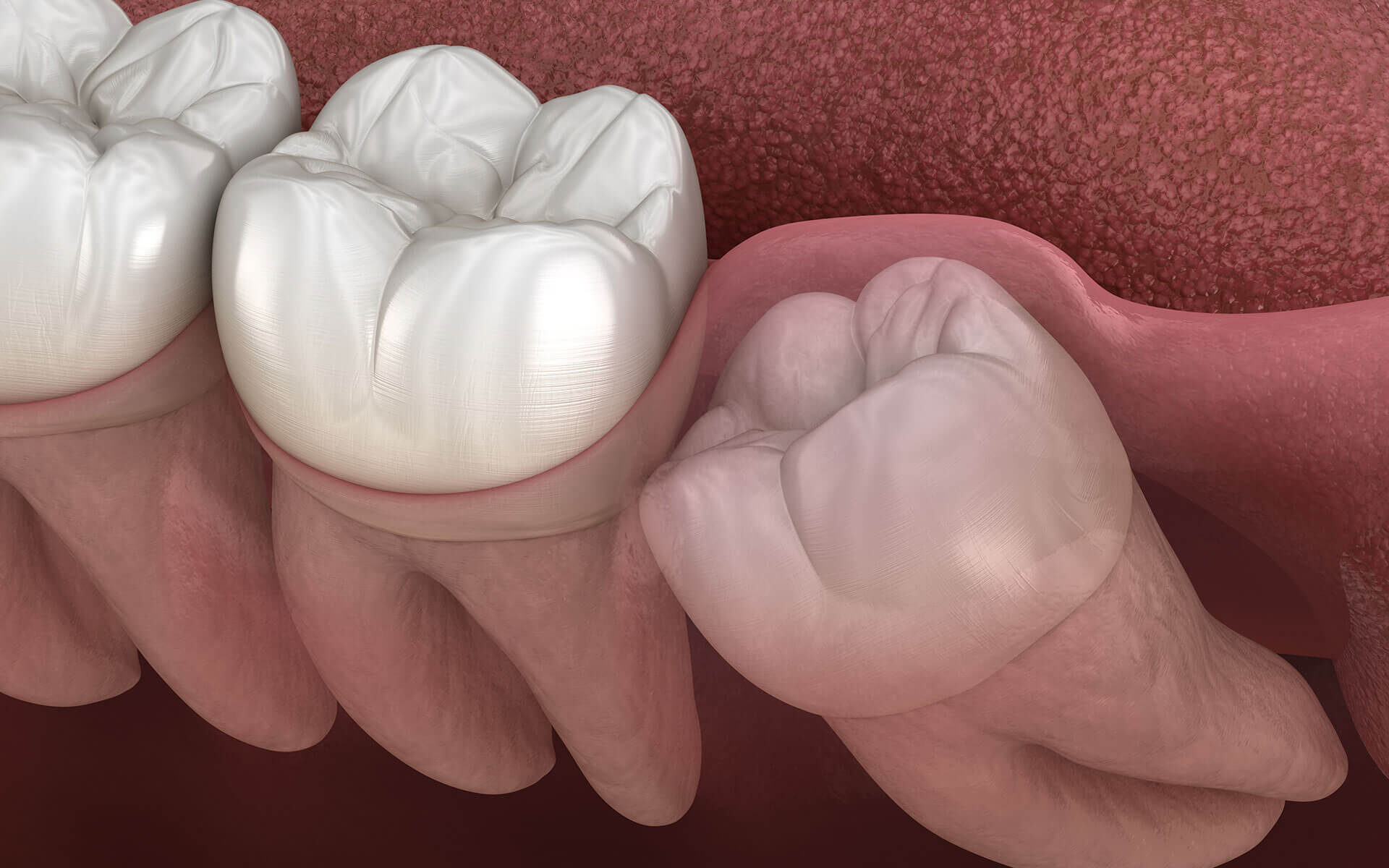
Unfortunately, many patients suffer from impacted or partially erupted wisdom teeth. This basically means the wisdom teeth refuses to erupt straight, and so, the wisdom teeth will erupt at an angle or potentially get stuck halfway. In some cases, your wisdom teeth, whether they have fully erupted or not, may be fine without any need for intervention. However, it is important to consult with your dentist to determine what your options are. The team at True Smiles Dental are well equipped to assess your wisdom teeth and give you an indication of what the best treatment options are for you and how to best prepare. In rare cases, patients may not present with wisdom teeth and all – The only way to figure that out is with an x-ray!
Why do the wisdom teeth erupt in such an odd manner? One theory suggests that due to our changing diet, humans are consuming more processed foods that don’t require as much chewing and tearing. This has possibly resulted in a reduction is jaw sizes with evolution. A smaller jaw is less accommodating for the eruption of all our teeth. And hence, wisdom teeth, which come out at a much later age, often do not have enough space to fully erupt. Although this is just one theory, the reasons for why wisdom teeth come out at a weird or funny angle is still uncertain. For the general populace, wisdom teeth should generally be removed for a number of reasons. We’ve listed a few of the common issues that are associated with wisdom teeth below:
1. Swelling
Swelling is commonly associated with wisdom teeth that have either erupted or partially erupted. The gum or fleshy part around the wisdom tooth can create a space for food and debris to trap under. Overtime, as the gums become irritated from the foreign debris – swelling, redness and pain can ensue. In most cases, food may dislodge itself and the issues resolve. Mouth rinsing or cleaning aids can be used to dislodge the debris. Although this may work in the early stages, overtime, the space may enlargen, making it trickier to remove debris that may trap itself underneath the gum.
Swelling can be painful and impact daily activities such as eating and talking. And in some severe cases, it can affect your mouth opening. If you notice a drastic increase in swelling size in a short period of time, we recommend you seek medical advice immediately.
2. Decay
Wisdom teeth don’t always erupt in the mouth straight and in line with the rest of your teeth. Impacted wisdom, or otherwise known as the ‘sideway’ wisdom teeth often find themselves trapping copious amounts of food between itself and the tooth in front (your second molar). Despite the best of intentions to keep the area clean, the deepest areas will tend to leave some food debris behind. And it is this food debris and its unwelcomed stay which is responsible for tooth decay. Our mouth has a finite amount of space, and our ability to keep all teeth clean can be quite difficult with teeth that are located further back in the mouth. As a result, our penultimate teeth, namely our second molars or wisdom teeth are often not kept as clean as we would like them to be.
Tooth decay can appear on either tooth, your wisdom tooth or the second molar tooth which lives in front. Unfortunately, decay that appears on the second molar tooth is difficult to detect without appropriate x-rays and close monitoring. Furthermore, should decay arise on the second molar tooth, the methods of treatment may be quite complex and costly due to the difficult nature of the decay. In some cases, the tooth may require root canal therapy, or even extraction due to the extensive tooth loss.
Should the decay affect the wisdom tooth, then treatment options generally recommend extraction of the wisdom tooth. In some circumstances, placing a filling on the tooth may be possible. A thorough exam of your teeth is highly recommended to detect any signs of decay on your teeth. Standard small film x-rays known as bitewings may not be enough to detect decay or issues with your wisdom teeth. An OPG (orthopantomogram) is recommended to assess the position of your teeth and its impact on neighbouring teeth.
3. Pain
Wisdom teeth can be quite troublesome when they start to erupt. Pain is often the first sign of your wisdom teeth coming through. Thankfully, the pain will dissipate with time as the wisdom tooth stops erupting. Unfortunately, we are unable to determine exactly when the wisdom tooth will stop erupting and, in some cases, wisdom teeth will continue to erupt throughout adulthood, and one may experience varying bouts of pain over a course of many years.
The pain you experience varies from individual to individual and is often dictated by the direction of your wisdom tooths eruption. The pain may inhibit eating properly as it can impact chewing or even talking. Over the counter pain relief medication may be useful for patients once wisdom teeth have started to erupt. If pain persists, we recommend seeking advice from your dentist.
Pain can be associated with infection, swelling, normal eruption, or complications associated with decay. Careful assessment with the team at True Smiles Dental, Marrickville can accurately determine what the issue is and can help you to devise a plan for treatment.
4. Infection or cyst formation
Infection is a complication that can be associated with swelling and pain. As mentioned previously, food can trap itself underneath the overlying gum tissue of your wisdom tooth. With time, swelling, pain and infection can develop. Infection in the area is when bacteria has multiplied and nestles itself underneath the gum tissue. Common signs include pus exudate which may be released upon pressure around the swelling.
In some circumstances, the infection can spread to more sinister areas and can result in facial swellings. Some infections can be slow and with the help of antibiotics, the infection may subside for a period of time. However, so long as the wisdom tooth remains, infection and swelling has the opportunity to return. We recommend removal of wisdom teeth that have experienced multiple bouts of infection to reduce the burden of constantly treating infections.
Cysts, are known as a sac like envelope that are often filled with fluid, air and other substances. Cysts can develop around wisdom teeth that haven’t fully erupted. So, even if you don’t see your wisdom teeth or haven’t had any issues with them, x-rays should be taken to determine whether there are any issues associated with your unerupted wisdom teeth. In rare instances, cysts may be present which require intervention with an Oral Surgeon. At True Smiles Dental, our new patient packages include an OPG x-ray, this allows us to carefully assess your entire jaw for abnormalities such as cysts.
5. Cheek biting and ulceration
Wisdom teeth have the tendency to not erupt fully, or often erupt at an angle. This can result to cheek biting which can be a painful experience, affecting talking and chewing. Cheek biting often develops into an ulcer, and the size of the ulcer can vary. Ulcerations can be quite painful and can take up to 2 weeks to heal.
We recommend an examination to identify the cause and suggest treatment options for the prevention of cheek biting and ulceration. Removal of your wisdom teeth may be indicated to prevent further cheek biting and mouth ulceration.
We’ve list 5 of the common issues that are associated with your wisdom teeth. Wisdom teeth issues have become ubiquitous amongst young adults, and we suggest patients receive thorough oral examination along with x-rays to determine the nature of your wisdom teeth. In some lucky individuals, they may not even have them at all, saving you the trouble of dealing with the above complications.
The team at True Smiles Dental, Marrickville are experienced in dealing with wisdom teeth complications and wisdom teeth removal. We employ the latest technology utilising 3D imaging to accurately assess your wisdom teeth for careful planning before removal. Are you experiencing any of the above complications? Call us on (02) 7228 7272, or book online at https://truesmilesdental.com.au/appointment